Frank Wheeler, OMS-IV
LECOM-Bradenton
Introduction
A middle-aged male complaining of resolved chest pain presents to the emergency department (ED). His physical examination is normal. His electrocardiogram (EKG) is seen in Figure 1 and cardiac enzymes were normal as well. The patient is determined to be low-risk for an adverse cardiac event and discharged home that night; however, two days later he returns to the ED. This time he arrives in cardiac arrest from a massive myocardial infarction. Reexamination of the EKG from two days prior reveals biphasic T waves in the precordial leads.
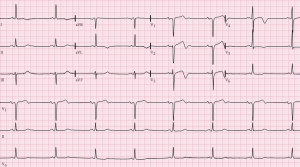
Figure 1 displays an electrocardiogram similar to this patient’s [1].
Background
This patient had Wellens syndrome. A syndrome that was incidentally found in 1982 by a group of cardiologists (including Dr.Wellens) who were studying the management of patients with unstable angina. Among 145 patients, 26 had similar T wave changes within the precordial leads, negative cardiac enzymes, and poor outcomes with conservative management. Eight of the first nine patients went on to develop anterior myocardial infarctions and three died. Ninety percent who underwent cardiac catheterization and coronary angiography were found to have greater than 90% stenosis in the proximal LAD. It was found that untreated Wellens syndrome has a high risk of myocardial infarction and death. The average time for infarction following EKG changes was days 1 to 23; with an average of 8.5 days [2].
In a second larger study, 180 out of 1260 unstable angina patients were found to have this syndrome. All were found to have at least 50% LAD blockage and 33 had complete occlusion. A number of these patients went on to develop anterior wall infarctions [3]. Wellens syndrome is therefore a pre-occlusion stage whereby acute myocardial infarction is imminent.
Characterization
Wellens syndrome can be identified most easily by its abnormal T wave findings in the precordial leads. These T wave abnormalities include either biphasic or inverted T waves. If one of these abnormalities are found, the patient must also have a history of anginal chest pain, but be pain free at the time of the EKG findings with normal or slightly elevated serum cardiac enzymes. Other ECG criteria for this syndrome also include a normal R progression without Q waves and ST elevation present [4]
Differential
Although T wave abnormalities are characteristic of Wellens syndrome, biphasic and inverted T waves can also be indicative of alternative diagnosis such as intracerebral hemorrhage, right bundle branch block, pulmonary embolism, hypokalemia, persistent juvenile T-wave inversion, or may be just a normal variant. Therefore, a finding of inverted or biphasic T waves can indicate a number of possible diagnosis and further history and clinical investigation is warranted to determine the cause.
Pathophysiology
Interestingly, the T wave abnormalities seen in Wellens syndrome are also seen in those who recently underwent reperfusion therapy following acute myocardial infarction [5]. It is therefore hypothesized that Wellens is an incidental reperfusion following occlusion of the LAD. The reperfusion may be unstable and this vessel may re-occlude, causing further angina and ischemia. This cycle of occlusion and reperfusion will continue until the coronary blood supply can no longer be reestablished and an acute myocardial infarction occurs.
Type of Wellens Syndrome
Currently two types of electrocardiographic findings for Wellens exist. Type A involves biphasic T waves in the precordial leads that begin positive then become negative, as demonstrated in Figure 2. This type is found less frequently than type 2 in around 25% of cases. Type B, which occurs in around 75% of cases, demonstrates inverted T waves (Figure 3) [6]. Throughout the cycle of occlusion and reperfusion that occurs over time, electrocardiographic findings will usually fluctuate through the different types of Wellens waves. However, if coronary supply is prone to worsen, EKG findings may show hyperacute T waves, indicating an anterior myocardial infarction. It is also important to note that Wellens syndrome does not always have to occur in the anterior leads but can also occur in other areas of the myocardium as well [7].

Figure 2 displays a Type A Wellens waves.

Figure 3 displays a Type B Wellens waves.
Management and Treatment
Patients with Wellens syndrome are to be treated as unstable angina. This includes aspirin, nitroglycerin, and pain control, if needed. Patients should be admitted to the hospital where serial cardiac markers and electrocardiograms should be followed. Interventional cardiology should also be consulted as early cardiac catheterization and intervention is imperative in Wellens syndrome [3,8]. With early recognition and proper intervention, usually PCI, the prognosis for Wellens syndrome is good. It is also important to note that stress testing is contraindicated in Wellens syndrome as the increase in myocardial demand can exacerbate the limited blood supply to the myocardium and precipitate a myocardial infarction [9].
Conclusion
Wellens syndrome is an important diagnosis to consider in a patient with T wave inversions or biphasic T waves and negative cardiac markers. Although these patients may be stable and pain free throughout their stay within the emergency room, a large number of patients will go on to experience anterior myocardial infarctions. With early recognition and intervention, significant morbidity and mortality can be avoided.
References
- Photo by Jer5150, distributed by a CC-BY-SA-3.0 licence (https://creativecommons.org/licenses/by-sa/3.0/deed.en). Accessed: 8/17/17. https://commons.wikimedia.org/wiki/File:Wellens%27_Syndrome.png
- de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103(4 Pt 2):730-6.
- de Zwaan C, Bär FW, Janssen JH, et al. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J. 1989;117(3):657-65.
- Rhinehardt J, Brady WJ, Perron AD, et al.. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med. 2002;20(7):638–43.
- Kosuge M, Kimura K, Nemoto T, et al. Clinical significance of inverted T-waves during the acute phase of myocardial infarction in patients with myocardial reperfusion. J Cardiol. 1995;25(2):69-74.
- Sz WHO, Khalighi K, Kodali A, et al. Omnious T-wave inversions: Wellens’ syndrome revisited. J Community Hosp Intern Med Perspect. 2016;6(4):32011.
- Agarwal A, Vyas S, Kumar R. Wellen’s syndrome: Challenges in diagnosis. Malays Fam Physician. 2015;10(3):35–7.
- Wang JY, Chen H, Su X, et al. Wellens’ syndrome in a 22-year-old man. Am J Emerg Med. 2016;34(5):937.e3-4.
- Sowers N. Harbinger of infarction: Wellens syndrome electrocardiographic abnormalities in the emergency department. Can Fam Physician. 2013;59(4):365-6.
